Haematology Watch, Vol 1, Issue 1.
CASE RECORDS
A young boy having fever and bleeding multiple sites
Dr. Mehmood-ul-Hasan, Dr. Nazia Khalid
A 15 yrs old boy was brought by parents from Tala Gang on 25.Oct.2008 to the emergency department of Fauji Foundation Hospital with the presenting complaint of:
-Fever…………….. 1 month
-Bleeding gums….. 15 days
-Blood in stool…….. 7 days
He was previously healthy, except for a tendency to heal poorly.
Fever was low grade, intermittent, not associated with shivering or sweating, or specific time of day, and it was not relieved by the medicines he took (i.e. Co-Amoxiclauv).
He also had developed gum bleeding and epistaxis, as well as blood in stool.
Otherwise, the Past Hx, the Family Hx, the Personal Hx, and the Social Hx were unremarkable.
A young boy with average built, co-operative, well oriented to time, place & person:
Pulse: 72/min
Temp.: 98 F
B.P.: 120/80 mmHg
B.R.: 18/min
Pallor: Positive
Jaundice/Clubbing/Cyanosis/Edema/ : Negative
Lymph nodes: Not palpable
G.I.T: Bleeding left sided gums
C.V.S./C.N.S./Resp. systems: Unremarkable
Temperature of 102F was noted. Cold sponging was advised.
PROVISIONAL DIAGNOSIS:
Pyrexia of unknown origin
Bleeding disorder
Following investigations were requested:
Blood CP/ESR Stool for occult blood
Urea/Creatinine Blood for M.P.
Electrolytes Blood for C/S
Stool and Urine R/E
PT, APTT
CXR
LFT & Hepatitis screening
Following treatment was started: Tab. ZANTAC (Ranitidine) 150 mg BD
Inj. TITAN (Ceftriaxone Na) 2 g BD
Inf. D/Saline 1000 cc OD
Inj. BEJECTAL (Vit.B1,B2,B6, Nicotinamide) OD
Tab. PARACETAMOL 1 SOS
Inj. NEUROBION (Vit. B1, B6, B12) OD
Tab. FOLIC ACID 5 mg OD
Inj. VITAMIN-K OD
TEST RESULTS: Hb: (g/dL) 15.3 3.2 4.4
RBC: (3.8-5.8 Х 1012 /L) 5.4 0.9 1.4
Hct: (%) 46.5 9.5 13
MCV: (fL) 85 102 94
RDW: 44 58 50
WBC: (/μL) 6500 1800 1290
[ANC]2000-7000 3700 576 230
[ALC]1500-3500 1950 774 695
[AMC]200-800 455 432 348
[AEC] 40-440 18
Platelets: 8 000/μL 2 000/μL 4 000 /μL
Creatinine: ( 60-156 μmol/L) 72 85
P.T.: 16/14 25/13 20/14
A.P.T.T. 39/28
Bilirubin: (<17 μmol/L) 5
A.L.T.: (U/L) 19 12
L.D.H.: (100-250 U/L) 368
Hepatitis B, C serology: Negative

He was transfused 1 unit R.C.C., 2 units Platelets, and 2 units F.F.P.
Pancytopenia due to Acute Leukemia or due to Aplastic anaemia was suspected.
Ultrasound abdomen was requested for status of abdominal viscera.
Simultaneously, Bone marrow examination was advised.

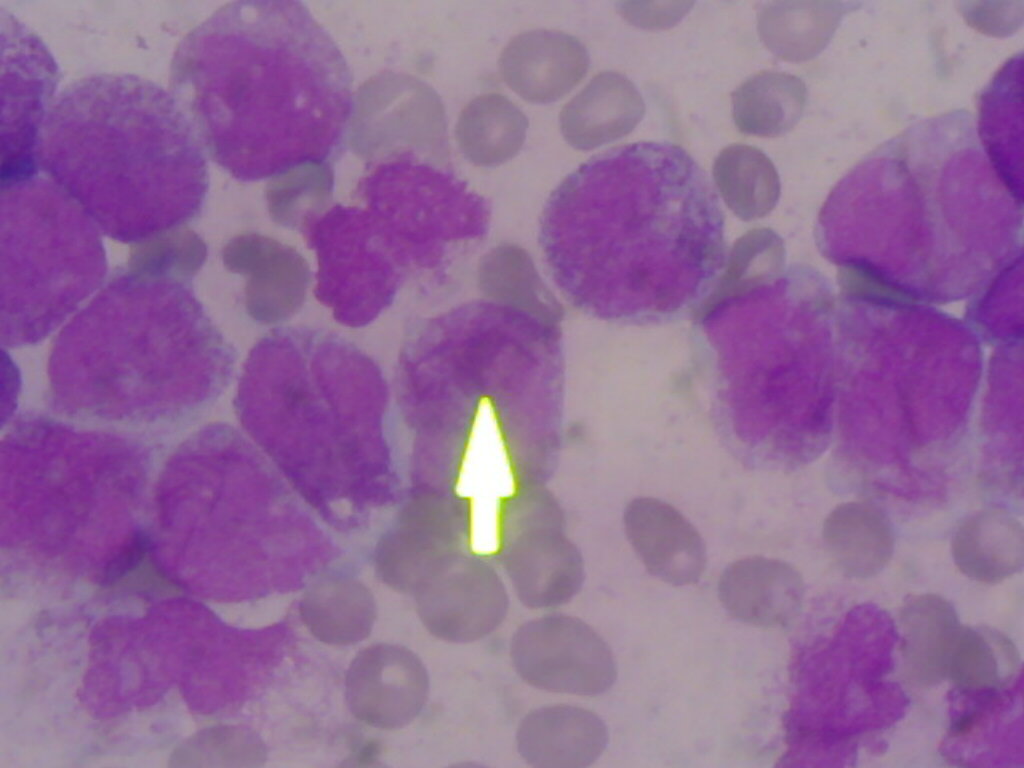
Referring to Peripheral blood smear and Bone marrow examination (Fig.1 and Fig. 2 below), a diagnosis of Acute Promyelocytic leukemia (FAB class AML M3) was made.
The next day his consciousness deteriorated, and multiple bruises at puncture sites developed.
Inj. GENTACIN (Gentamycin), Inj. AUGMENTIN (Co-amoxiclauv), Inj. TRANSAMIN (Tranexamic acid), and O2 INHALATION was started.
Following investigations were requested:
F.D.P.s (D-dimers) for DIC
Serology for Dengue fever (Ig M)
Coagulation profile (INR, APTT, Fibrinogen)
Sohail Khan died on 3rd day of admission (27th October) at 8 pm.
Following were his awaited lab. reports:
MP: Not seen
Blood C/S: No growth
FDPs: Pending
Stool for occult blood: Pending
Stool R/E: Pending
Urine R/E: Pending
DISCUSSION
Acute myeloid leukemias affects all age groups, but are increasingly common with progressing age.
The most common genetic abnormality is presence of internal tandem repeats of the FLT-3 gene whose expression is normally tightly regulated in CD34+ cells.
FAB classification- M0: Minimally differentiated acute myeloblastic leukemia
- M1 : Acute myeloblastic leukemia without maturation
- M2: Acute myeloblastic leukemia with granulocytic maturation
- M3 : Acute promyelocytic leukemia (APL)
- M4 : Acute myelomonocytic leukemia
- M4eo : Myelomonocytic together with bone marrow eosinophilia
- M5 : Acute monoblastic leukemia (M5a)
- M6: Acute erythroid leukemia, including erythroleukemia (M6a) and very rare pure erythroid leukemia (M6b)
- M7 : Acute megakaryoblastic leukemia
WHO classification
[attempts to be more clinically useful and to produce more meaningful prognostic information than the FAB criteria]
AML with characteristic genetic abnormalities:
[t(8;21)], [inv(16)], or [t(15;17)]
a high rate of remission
better prognosis compared to other types of AML.
AML with multilineage dysplasia:
prior MDS or MPD transforming into AML.
most often in elderly
worse prognosis.
AML and MDS, therapy-related:
prior chemotherapy and/or radiation and subsequently develop AML or MDS.
may be characterized by specific chromosomal abnormalities,
worse prognosis.
AML not otherwise categorized:
subtypes of AML that do not fall into the above categories.
Acute leukemias of ambiguous lineage:
(also known as mixed phenotype or biphenotypic acute leukemia) occur when the leukemic cells cannot be classified as either myeloid or lymphoid cells, or where both types of cells are present.
In normal haematopoiesis, the myeloblast is an immature precursor of myeloid white blood cells.
In AML, a single myeloblast accumulates genetic changes which "freeze" the cell in its immature state and prevent differentiation. When such a "differentiation arrest" is combined with oher mutations which disrupt genes controlling proliferation, the result is AML.
Heterogeneity of AML is due to transformation at a number of different steps along the differentiation pathway.
The types of chromosomal abnormalities often have prognostic significance. The chromosomal translocations encode abnormal fusion proteins, usually transcription factors whose altered properties may cause the "differentiation arrest." For example, in Acute Promyelocytic leukemia, the t(15;17) translocation produces a PML-RARα fusion protein which binds to the retinoic acid receptor element in the promoters of several myeloid-specific genes and inhibits myeloid differentiation.
As the leukemic clone of cells grows, it tends to displace or interfere with the development of normal blood cells in the bone marrow.
DIC and AML-M3:
- Pro-coagulant granules released from promyelocytes
- Bleeding from venepuncture sites
- Intracranial bleed
Role of All-trans retinoic acid:
- It converts transcription repressors to transcription activators thus resulting in a cellular program for differentiation to mature cells.
- Although a remission can often be induced with ATRA alone, combining it with chemotherapy (usually daunorubicin and cytarabine) gives better long-term results.
- The side
effects include retinoic
acid syndrome, i.e. breathing problems due to fluid buildup in the
lungs, low blood pressure, kidney damage, and severe fluid buildup elsewhere in
the body. It can often be treated by stopping the ATRA for a while and giving
dexamethasone. During
treatment, some patients with APL may also develop blood-clotting problems.
They may be given an anticoagulant ("blood thinner") to help prevent
or treat this.
References:
Essential Haematology by Hoffbrand
Wang, Zhen yi, International Bibliographic Information on Dietary Supplements
Fig. 1. Peripheral blood smear of AML-M3
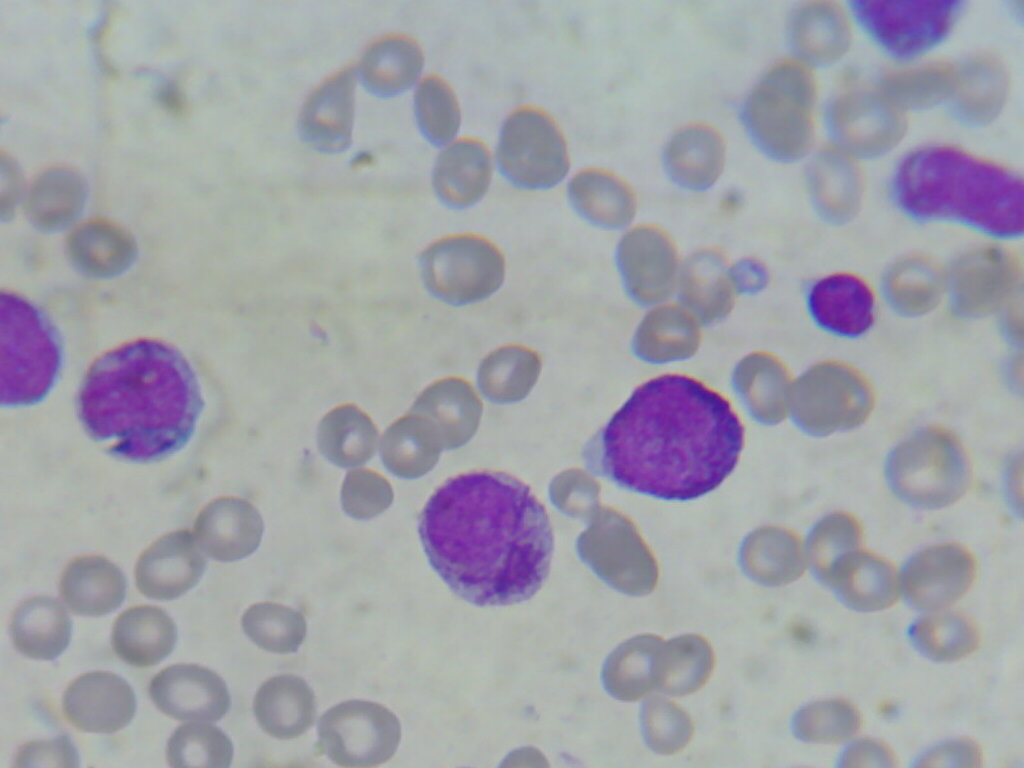
Fig. 2. Bone marrow aspiration slide of AML-M3