Haematology Watch, Vol 3, Issue 1.
BASIC HAEMATOLOGYSpherocytes and irregularly contracted cells
Barbara J. Bain
There are three types of cell that appear hyperchromatic on a blood film and have an increased concentration of haemoglobin detectable on automated instruments (MCHC increased). They are spherocytes, microspherocytes and irregularly contracted cells (ICC). The difference between ICC and spherocytes/microspherocytes was recognised by the late Professor Sir John Dacie who used the designation ‘spherocyte-like cells’ for ICC. Spherocytes and microspherocytes have a regular outline and lack central pallor. ICC also lack central pallor but have an irregular outline. They can reasonably be described as ‘contracted’ since their volume is reduced and they have an increased mean cell haemoglobin concentration. Since the differential diagnosis is quite different (Table), it is important to distinguish between spherocytes and irregularly contracted cells.
Table Principal causes of spherocytes and irregularly contracted cells
Spherocytes | Irregularly contracted cells |
Hereditary spherocytosis | Oxidant stress in glucose-6-phosphate dehydrogenase deficiency or other defects of the pentose shunt |
Immune haemolytic anaemia ― autoimmune haemolytic anaemia, alloimmune haemolytic anaemia (delayed transfusion reaction, haemolytic disease of the newborn, administration of anti-D to Rh D-positive subjects) | Severe oxidant stress (drugs or chemicals) in individuals with normal red cell enzymes |
Red cell fragmentation syndromes (microangiopathic haemolytic anaemia and mechanical haemolytic anaemia) | The presence of haemoglobin C, haemoglobin E or an unstable haemoglobin |
Spherocytes (Figs 1 and 2) result from loss of membrane in excess of loss of cytoplasm, either through the action of macrophages of the reticuloendothelial system or through fragmentation in the circulation.
Fig. 1: Hereditary spherocytosis showing numerous spherocytes, some of which are indicated by an arrow.

Fig. 2: Autoimmune haemolytic anaemia showing numerous spherocytes, some of which are indicated by an arrow.

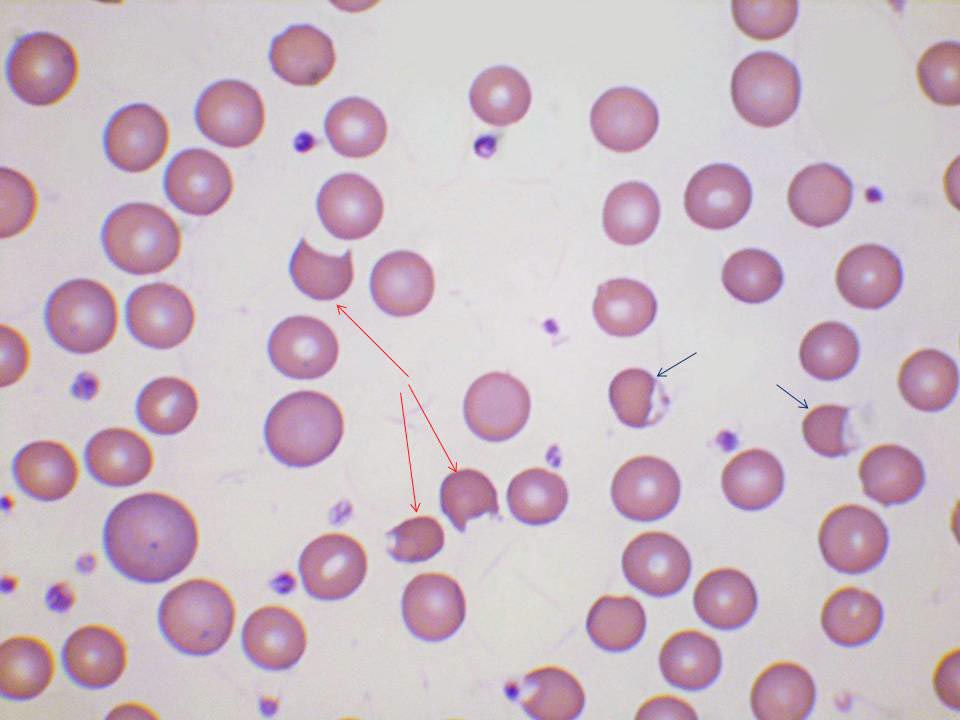
Irregularly contracted cells result either from (i) oxidation of haemoglobin, the red cell membrane and other cellular constituents or (ii) the precipitation of a variant haemoglobin that is unstable or has reduced solubility. When ICC result from oxidant damage, other abnormal cells are likely to be present including keratocytes (from which a Heinz body has been removed) (Fig. 3), hemighosts and ghost cells.
Fig. 3: Glucose-6-phosphate dehydrogenase deficiency showing irregularly contracted cells (black arrows), keratocytes (red arrows) and polychromatic macrocytes
When due to an unstable haemoglobin (Fig. 4) there may also be keratocytes and polychromasia.
Fig. 4: Irregularly contracted cells (arrows) in a patient with haemoglobin Köln, an unstable haemoglobin.

When due to homozygosity for haemoglobin C there is a mixture of ICC and target cells, while in compound heterozygosity for haemoglobin C and either beta0 or severe beta+ thalassaemia (Fig. 5) there is also hypochromia. Heinz bodies are detectable when ICC are due to acute oxidant damage and the term ‘Heinz body haemolytic anaemia’ is sometimes used. Depending on the severity of the haemolysis and the effectiveness of the spleen at removing them, Heinz bodies may also be detected in patients with an unstable haemoglobin.

.
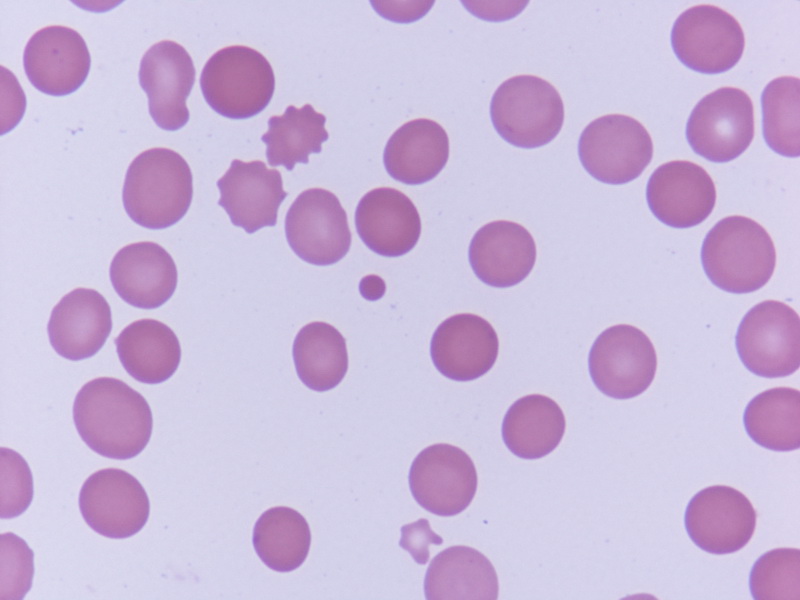
Microspherocytes are seen in severe fragmentation syndromes including some instances of microangiopathic haemolytic anaemia (Fig. 6); in this case there are also schistocytes (angular red cell fragments). Microspherocytes can be regarded as spheroschistocytes since they inevitably result from fragmentation of a red cell. Microspherocytes are also seen in burns, when they result from budding off of fragments of red cells. In patients with burns there are also spherocytes and microdiscocytes (red cell fragments that maintain their central pallor).
Fig. 6: A microspherocytes in a patient with a microangiopathic haemolytic anaemia. (Photograph by courtesy of Dr Abbas Hashim Abdulsalam, Al-yarmouk Teaching Hospital, Teaching Laboratories Department, Haematology Unit, Baghdad.)
Barbara J. Bain
Professor of Diagnostic Haematology,
Imperial College Faculty of Medicine,
St Mary’s Hospital,
London.