Haematology Watch, Vol.5, Issue 2.
LABORATORY HAEMATOLOGY
Coombs Test: Interpretation
Mehmood
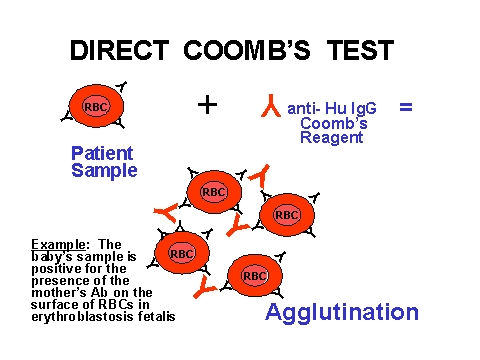
Direct Coombs Test
Direct Coombs test detects antigen/antibody on RBC of patient. When performed according to the standard operating procedure (SOP), it is quite a useful test.
Image 1.0 (http://newborns.stanford.edu/Coombs.html)
False Negative Coombs test:
1. If a Coombs test is negative, it means that either it is true negative or a false negative. A false negative means that the Coombs reagent has attached to some thing other than the target on RBCs. This means that the attaching of Coombs reagent to such a thing e.g. an antibody in plasma present around RBC is a phenomenon which can not be appreciated due to absence of any agglutination. Thus, when RBCs will not be washed properly, an antibody on RBC will remain unattached by Coombs reagent because before the reagent attaches to RBCs, plasma containing an antibody intervenes thus inhibiting contact of Coombs reagent with RBCs having antibody on their surface.
To resolve this, add Check cells in the test sample tube. If Coombs reagent is truely working and presence of plasma is the culprit, the Check cells will be agglutinated, leading to a positive result. If this does not happen, the Coombs reagent is faulty.
2. Delay in adding Coombs serum after washing step will lead to antibody eluting off, detaching from cell, while cells are sitting in saline. Now free antibody present in the saline neutralizes the Coombs serum so it will not be able to react with the cells bound with antibody.
3. Small fibrin clot among the cells that were not washed away will have immunoglobulins and complement present. The antibodies and complement in the fibrin clot neutralizes Coombs serum leading to a negative test.
4. Inactive Coombs serum or the failure to add Coombs serum will also be detected by a negative reaction when adding Coombs Control Check Cells.
There are also false negatives NOT detected by negative Coombs Check Cells that include:
5. Too heavy cell suspension6. Delay during cell washing procedure, which can lead to antibody eluting off cells while they are sitting in saline and then the antibody is washed away during the remaining washes
7. Improper centrifugation can either lead to loss of cells during washing or the need to shake too hard during resuspension.
False Positive Coombs test:
1. Using improper specimen (clotted instead of EDTA-anticoagulated for Direct Coombs Test)
2. Spontaneous agglutination (cells heavily coated with IgM)
3. Non-specific agglutination ("sticky cells")
All of these reactions would be the result of cells appearing to agglutinate, or actually agglutinating. Using a clotted tube for the DAT may allow complement to become activated in the test tube since calcium ions are free to be part of the complement cascade.
Clinical Interpretation of A Positive Coombs test:
1. Normal patient with unexplainable reasons for a positive DAT
2. Transfusion reaction work-ups require that a DAT be performed on the post-transfusion specimen since the patient's antibodies and/or complement may coat the transfused donor cells. These reactions are usually a weak positive or mixed field agglutination since you are testing a mixed population of patient and donor cells.
3. Warm-acting Autoimmune disease can lead to patient antibodies coating their own cells. This results in a strong positive result. A cold-acting autoimmune haemolytic anemia would be due to IgM antibodies that activate complement. The complement-coated cells would then be detected by the Coombs reagent.
4. Hemolytic disease of the newborn is due to the mother's IgG antibodies crossing the placenta and coating the antigens on the fetal red blood cells. Cord blood collected at the time of birth would be tested, but may need to followed up by a heel stick of EDTA blood. The reaction is usually a strong positive.